
What is IBS?
Irritable Bowel Syndrome or IBS is a chronic condition that can affect up to 10-20% of people at some point in their life. Monash University in Australia believes that 1 in every 7 adults suffers with IBS. Symptoms include abdominal pain and discomfort, bloating, wind, distension and altered bowel habits (ranging from diarrhoea to constipation), but often no altered pathology is seen in the digestive tract. This article will cover the main causes of IBS and what we can do about it.
Rather than being a specific disease, IBS is actually a cluster of symptoms which can make life very challenging for the sufferer as day-to-day life can be so unpredictable. It is common for bouts of IBS to be accompanied by fatigue.
Although GPs and Doctors are managing to diagnose IBS more quickly, there is no standard treatment for the condition, which can leave many patients feeling let down and frustrated. This is partly because there is no single cause, but rather several triggers that can make the condition worse.

The Common Causes of IBS:
- Stress. The gut has its very own nervous system called the ENS (enteric nervous system). Although this can work independently from the brain, feelings of being stressed or anxious can affect the normal nerve signals in the gut. This connection which can become disrupted is known as the brain-gut axis.
- Lactose or fructose intolerances. Although food intolerances can affect the immune system, a food intolerance usually refers to a condition where the body is lacking an enzyme to digest certain molecules or where there is malabsorption.If we struggle to digest lactose or fructose, these molecules may ferment in the bowel, leading to distention and pain. Examples are lactose intolerance or fructose malabsorption.
- Food Allergies. Surprisingly this is not one of the main reasons for IBS, however symptoms can be severe in the case of wheat or gluten. Allergies can affect either IgE or IgG mediated. Food allergy symptoms are therefore by no means limited to the gut, although they can lead to inflammation of the delicate gut lining and contribute to pain and gut permeability.
- Certain foods are also known to irritate the condition, especially foods that contain high levels of fermentable carbohydrates, that we call FODMAPS. These foods do not cause IBS, but can exacerbate symptoms. They can range from many fruits and vegetables, dairy products, legumes, nuts and seeds as well as some alcoholic drinks and sweeteners. (See later for more information on the FODMAP diet).
- Hormones. Many women find that symptoms worsen around the time of their monthly period so cycle mapping can be helpful.
- Medicines. Certain medications such as anti-inflammatories and painkillers can induce IBS like symptoms, as can certain iron supplements. In addition, supplements that use sorbitol to sweeten them, may induce IBS symptoms. Codeine and other morphine-based painkillers are well known for causing constipation and may slow down transit time considerably.
- Gut dysbiosis (imbalance of healthy bacteria).
Bacteria in our gut outnumber our human cells and we can have up to 10-100 trillion microbes in a healthy gut microbiome. They are vital to our health and are mostly symbiotic. This means that they live within us, but both bacteria and man benefit from this co-habitation.
Widespread antibiotic use, poor diet, inferior digestion and an unhealthy lifestyle can mean that the gut flora can become disrupted. Higher amounts of fermentation bacteria, yeasts and even protozoans may therefore inhabit our intestines. The result is a gut that is prone to fermentation of the food we eat. Fermentation can produce large amounts of gas which often leads to pain and diarrhoea.
- Altered Gut Motility – where the contents of the gut move too fast or too slowly through the gut.
- SIBO (small intestinal bacteria overgrowth) Small intestine bacterial overgrowth or SIBO is where unusually high numbers of bacteria are present in the small intestine where the food is broken down and absorbed. These bacteria can encourage fermentation of undigested food causing high levels of gas (hydrogen, methane of hydrogen sulphide). Fungal infections and yeasts may be implicated in this condition.
Only small amounts of bacteria should be present in the small intestine, with the large majority inhabiting the large intestine. Abnormally high numbers of bacteria this part of the gut that can become problematic to our digestion. Whereas bacteria in the large bowel usually feast on vegetable fibres and undigested food particles, bacteria in the small intestine have access to increased levels of carbohydrates which can encourage fermentation and gas production. - Post Infectious Irritable Bowel Syndrome. This can occur after what appears to be a bout of infection in the stomach and intestines (gastroenteritis) and is termed post-infectious IBS (PI-IBS).Certain infections such as Campylobacter jejuni, Salmonella, Shigella as well as Giardia and E.coli are the most common. Although the symptoms of these infections may only last a few days, the disruption to the gut’s microbiota (gut bacteria) can persist for months and often years afterwards. Sometimes the nerves lining the small intestine can be affected resulting in the motility and contraction function, known as the MMC (migrating motor complex) being disrupted. The migrating motor complex helps to flush bacteria and food remnants out of the small intestine and into the large intestines at the end of the day and sometimes between meals as a self-cleaning response.
Other IBS related conditions that may mimic IBS:
- Coeliac disease is a severe auto-immune condition where the body reacts very strongly to minute amounts of gluten in the diet. The body responds by attacking the lining of the gut which damages the microscopic villi that are essential to a healthy digestion. This may be mistaken for IBS, however this is a severe medical condition that requires a strict gluten-free diet.
- Inflammatory bowel disease (IBD). IBD is different from IBS and, like coeliac condition is a severe inflammatory condition. Any type of inflammatory bowel disease can be mistaken for IBS. IBD normally includes colitis (usually large intestine) and Crohn’s disease (small intestine). IBD leads to chronic inflammation of the gut.
- Parasites. Some parasites can mimic symptoms of IBS and lead to intestinal symptoms.
- Bile Acid Malabsorption. This is a condition where bile acids are not reabsorbed in the colon correctly and instead can lead to watery stools and diarrhoea.
- Histamine intolerance. Sometimes symptoms of histamine intolerance can mimic IBS. Histamines are more commonly associated with skin (itching, urticaria and hives), but can also lead to Gastrointestinal discomfort.
Main Symptoms of IBS
The main symptoms of IBS are bloating and distension. This can lead to abdominal pain and discomfort with a feeling of increased pressure in the abdomen. These symptoms typically increase after food. It can be difficult to differentiate where pain in the gut is coming from.
Most of the symptoms and pain can be linked back to bloating and distention, of which there are just 3 main causes.

Different types of IBS
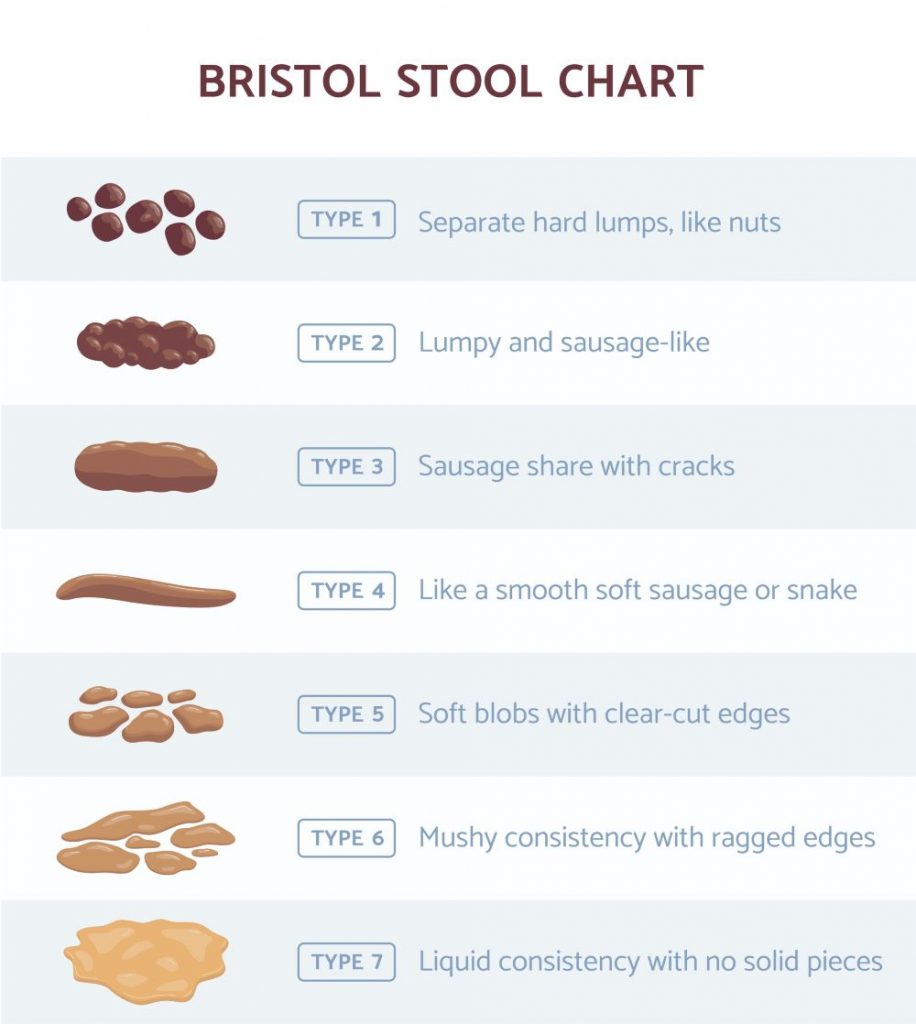
There are 3 different ways in which IBS occurs. One symptom may be more prominent than others, while other symptoms may occur more randomly or unpredictably. These bowel experiences and their unpredictability can lead to a high degree of anxiety for the IBS patient. External factors, such as stress, can also affect stool consistency. IBS has different sub-groups, which are associated with stool consistency.
- IBS-D is when our digestive system contracts quickly, transiting products of digestion rapidly through the digestive tract, resulting in frequent, watery bowel movements (diarrhoea).
- IBS-C is when our digestive system contracts more slowly, delaying transit time for products of digestion, resulting in hard, difficult to pass, infrequent stools (constipation).
- IBS-M is when our transit time throughout the digestive tract fluctuates, causing us to experience a mix of both diarrhoea and constipation, often alternating between the two. These extreme stool consistencies can sometimes even occur within the same bowel movement.
Intestinal pain can occur when material in one section of the gut passes through slowly while material in another section passes through quickly. These simultaneous actions can produce bowel movements alternating between constipation and diarrhoea, sometimes within the same bowel movement. In addition, prolonged contractions of the bowel might prevent the normal passage of air and trigger bloating, wind, and flatulence. Bloating could become so severe that clothing feels tighter and abdominal swelling becomes visible to others.
Bowel movements – what is normal?
Stool consistency may vary enormously, ranging from entirely liquid to so firm and separated that it resembles small pebbles in IBS. It is normal to expel a stool up to 2-3 times a day, however most people rarely manage this. The amount of stool should be around the length of our wrist to our elbow daily. A stool should be brown in colour and should form a soft sausage shape. It is normal for small undigested seeds, tomato skin and corn kernels to be present in the stool. The Bristol stool chart has kindly assigned a scale to different stools. We are aiming for a number 4!
Improving IBS with diet and lifestyle
The following lifestyle changes may help to reduce the symptoms of IBS in many individuals.
- Food should be eaten slowly and chewed properly. Bolting food will make symptoms worse
- Avoid large portion sizes at meals, but equally try not to snack continuously during the day. This will give our gut a better chance of digesting the food fully, which can, in turn reduce fermentation.
- Avoid rich and oily foods which can increase pain and discomfort
- Caffeine is a stimulant that can speed up transit time. If you suffer from constipation this may be beneficial; however, it can worsen symptoms in those with diarrhoea
- Alcohol has been shown to worsen IBS. Limit alcohol consumption to 1 drink 2-3 times a week and avoid alcohol on an empty stomach.
- Eat regularly and avoid skipping meals
- Drink around 2-2.5 litres water daily
- Be aware of your stress triggers and try to avoid stress at mealtimes.
- Exercise can encourage a healthy peristalsis (movement in the gut) and can help to normalise bowel movements. Running, however, can put an increased strain on the gut and may increase diarrhoea symptoms.
Does wheat or gluten cause IBS?
Many people with IBS believe that they are allergic to gluten, but it is not that straightforward! An allergy to gluten can be linked to undiagnosed coeliac disease or non-coeliac gluten sensitivity. However, most people with IBS are actually reacting to a smaller part of the wheat known as fructans. Fructans are part of the FODMAP family and are carbohydrate molecules that are difficult for us to digest. Gut microbes however love to feast on fructans and can produce gas as a bi-product leading to bloating, gas, pain and sometimes diarrhoea. Eating gluten-free may alleviate some of the symptoms, but it is often a fermentation problem, rather than an allergic reaction involving our immune system.
What about the FODMAP diet?
The FODMAP diet is an acronym for Fermentable Oligosaccharides, Disaccharides, Monosaccharides and Polyols. These are the hard to digest carbohydrate molecules that are present in a myriad of foods from wheat, onions, garlic, beans and lentils, certain fruits, such as apples and bananas, honey, certain vegetables, and some dairy. This diet can be helpful in working out which foods are triggering the most symptoms. It is not a cure for IBS as some people believe, but rather a diagnostic tool. See below.
Can Diet Help Resolve IBS?
A series of diet and lifestyle measures work best when working through IBS as we also need to work on the underlying cause. As a nutritional therapist, my aim is to work upstream of the symptoms to help my clients get long lasting results. Sometimes it is necessary to carry out testing to help identify the problems, so some or all of the following would be taken into account.
- Laboratory testing
- Such as Stool or SIBO testing may be required to isolate the root cause.
- Occasionally food allergy testing may be recommended.
- A low fermentable diet, such as FODMAP may be recommended for a short period (no more than 6 weeks to identify triggers.) *This should be carried out under the supervision of a nutritionist/ nutritional therapist/ dietician. Reintroduction is crucial.
- Rebalancing of the gut microbiome to build resilience. This may involve:
- Increasing and supporting healthy gut microbes
- Reducing inflammation
- Encouraging healing of the gut membrane
- Supporting digestion
- Supporting/ slowing motility
- Reducing frequency with diarrhoea or increasing motility for constipation.
- Addressing parasites/ SIBO
- Using targeted supplements/ antimicrobials where appropriate.
*The FODMAP diet has been developed by scientists at Monash University in Melbourne which has been successfully adapted by UK researchers at King’s College London. The FODMAP should only be carried out under the supervision of a nutritionist/ nutritional therapist/ dietician for a SHORT period of time only!

What to Do if You Think You Have IBS
Always consult a medical professional in the first instance to determine whether a diagnosis of IBS is correct and to rule out other causes. It is also advisable to seek advice from a qualified nutritionist / nutritional therapist who can help to identify your triggers using a combination of personalised nutrition or advanced laboratory testing to help identify triggers and to find the right nutrition programme for you.
Dominique Ludwig is the author of this article and as a qualified Nutritionist and Nutritional Therapist, has helped many patients with IBS symptoms during her 20 years of clinical experience. Do get in touch with Dominique for a discovery call if you think you would like advice on how to relieve your IBS symptoms through diet.
To take the first step, why not book a discovery call with Dominique Ludwig BOOK A DISCOVERY CALL HERE
DISCLAIMER:
Features published by Dominique Ludwig are not intended to treat, diagnose, cure or prevent any disease. Always seek the advice of your GP or another qualified healthcare provider for any questions you have regarding a medical condition, and before undertaking any diet, exercise or other health-related programme.




